 Patients with diabetes mellitus cannot use and store sugar properly. High blood sugar levels result, which can cause damage to blood vessels throughout the body, including the blood vessels that supply the retina. The retina is critically important in vision. It is the nerve layer in the back of the eye which send signals to your brain for sight to occur. This damage to these retinal vessels is called diabetic retinopathy. People with diabetes have an increased chance of developing a variety of additional eye problems, including cataracts and glaucoma.
Patients with diabetes mellitus cannot use and store sugar properly. High blood sugar levels result, which can cause damage to blood vessels throughout the body, including the blood vessels that supply the retina. The retina is critically important in vision. It is the nerve layer in the back of the eye which send signals to your brain for sight to occur. This damage to these retinal vessels is called diabetic retinopathy. People with diabetes have an increased chance of developing a variety of additional eye problems, including cataracts and glaucoma.
In most cases, the effect of diabetic retinopathy on the retina is an extremely serious threat to vision. Many patients who have been diabetic over 5 years have retinopathy already and as many as one in five have it diagnosed during their comprehensive eye examination. While it is true that there is no cure for diabetes, diabetic eye care from Kaufman Eye Institute physicians provides treatment options to prevent serious complications.
Types of Diabetic Retinopathy
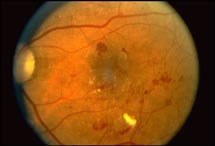
There are two main types of diabetic retinopathy. In the early stages of this disease the vessels become weak and leak. This earlier stage of diabetic eye disease is called background retinopathy or NPDR by eye doctors (non-proliferative diabetic retinopathy). In this stage, the weak vessels leak blood and fluid into the retinal layers which can cause the retina to swell or form deposits called exudates.
Proliferative diabetic retinopathy (PDR) is the much more serious evolution of diabetes in the eye. PDR occurs when abnormal new vessels (neovasculization) begin to grow on the surface of the retina (NVE) and/or the optic nerve (NVD). The main reason that this happens in widespread closure of fine retinal vessels which prevents adequate blood flow and circulation to the tissue. The eye responds by growing new blood vessels in this area in an attempt to resupply circulation to the area. Unfortunately, the new abnormal blood vessels do not resupply the retina with normal blood flow and are very weak. These vessels can also be accompained by scar tissue formation which contracts and causes wrinkling or detachment of the retina.
Can my lifestyle make a difference in treating diabetic eye disease?
Your lifestyle plays a huge role in the progression of the diabetes.
- Eat healthy and follow strict diabetic diet guidelines to control your sugar.
- Don't smoke.
- Maintain normal blood pressure.
- Watch your weight.
- Keep regular visits with your primary care doctor and take medications appropriately that he or she prescribes.
- Exercise.
Eye complications from Diabetic Retinopathy
There are many eye disease complications that occur during the development of diabetic retinopathy. The following is a summary of these complications in their major categories.
Macular Edema
Macular edema is the swelling or thickening of the macula (the center of the retina), which gives your best vision. The swelling is caused by the leaking of blood and fluid from leaky vessels around this area and is the most common cause of vision loss from diabetes. The vision loss can be mild or severe and treatment is important to retain function when it occurs.
Vitreous Hemorrhage
Sometime fragile new blood vessels in the eye bleed. Since these vessels are on the surface of the retina, they bleed into the clear jelly of the eye called the vitreous. If the hemorrhage is small, a person may only get a few symptoms of floaters. However, if the hemorrhage is large, than a patient may have a severe darkening of their vision where the hemorrhage is located.
It may take weeks to months for the eye to reabsorb the blood depending on how much is present and the status of the patient's diabetes. If the eye does not clear adequately on its own, laser technology or surgical intervention called a vitrectomy may be needed.
Traction Retinal Detachment
When PDR is present, scar tissue associated with new blood vessels (neovascularization) can shrink and contract, pulling the retina off it's normal position. Distortion from this wrinkling, if near the macula, can cause distortion in the vision as an initial symptom. More severe loss will happen in the macula or other areas of the retina if they detach.
Neovascular Glaucoma
Sometimes the process of retinal vessel closure from diabetes causes new abormal blood vessels to grow not only on the retina, but the iris (the colored part of the eye) as well. Drainage channels out of the eye get blocked as these vessels grow so that fluid cannot naturally drain out of the eye. Pressure in the eye builds up and causes a very serious type of glaucoma called neovascular glaucoma. This disease can cause extreme pressure in the eye which will damage the optic nerve and cause irreversible loss of vision.
How is diabetic retinpathy diagnosed?
A comprehensive medical eye examination is crucial to properly diagnose diabetic retinopathy. Kaufman Eye Institute physicians can often diagnose and treat serious reinopathy before you are even aware that the disease exists in your eyes. The EyeMD will dilate your pupil and look inside the eye with special equipment and technology to assess this serious condition.
If retinopathy is found, an additional specific test to assess the situation may be required. This test includes digital photography of the eye called fluorescein angiography to determine if you need treatment. Also, a new advanced technology called ocular coherence tomography can be used to safely section retinal tissue with a scanning laser to further assess your eyes and pinpoint where fluid may be leaking.
Diabetic Retinopathy Treatment
There is no cure for diabetic retinopathy. The best thing that a patient can do is to prevent retinopathy as much as possible. Strict control of your blood sugar will significantly reduce the long-term risk of vision loss. Unfortunately, In many cases the Kaufman Eye Institute physicians must treat your disease to prevent serious vision loss and may treat macular edema with injections of medicine in your eye. The special injections contain medicine with either steroids or other medications to shrink the swelling of the macula and other retinal tissue.
Laser Surgery
Laser surgery is commonly used in the treatment of diabetic eye disease. It is often used for patients with diabetic macular edema, proliferative diabetic retinopathy and neovascular glaucoma.
For diabetic macular edema the laser is typically focused in a special grid pattern around the macula to decrease fluid leakage. The goal of treatment is to prevent further loss of function of the macula and to attempt to recover vision by reducing the edema or swelling.
For PDR, the laser is focused on sections of the retina except the macula. This laser technique is called panretinal photocoagulation. It is usually effective in shrinking abnormal blood vessels and preventing them from growing in the future. It also decreases the chance that vitreous bleeding will occur.
Vitrectomy Surgery
Vitrectomy is a surgical technique that is sometimes required in severe cases of diabetic eye disease. During this microsurgical procedure, the blood-filled vitreous is removed and replaced with a clear solution. Vitrectomy often can prevent further bleeding by removing these abnormal vessels that cause the bleeding. It can also be used to relieve macular traction from scar tissue so that it is not distorted. The longer the macula is distorted or out of place, the more serious the vision loss will be.


